No scalpel vasectomy has transformed male sterilization by offering a minimally invasive, highly effective procedure with faster recovery and fewer complications. While surgical technique plays a crucial role in these improved outcomes, optimal results depend just as much on what happens after the procedure. This is where targeted post-op care plans become essential. Rather than relying on one-size-fits-all recovery advice, modern no scalpel vasectomy emphasizes personalized, evidence-based post-operative care tailored to each patient’s needs.
Understanding how no scalpel vasectomy and targeted post-op care plans work together helps patients recover more comfortably, avoid complications, and return to daily life with confidence.
Why Post-Op Care Matters in No Scalpel Vasectomy
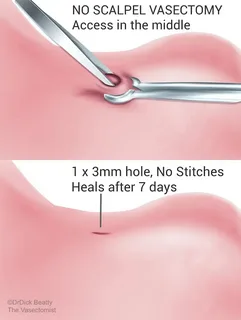
No scalpel vasectomy (NSV) minimizes tissue trauma by using a small puncture instead of surgical incisions. This approach reduces bleeding, swelling, and infection risk. However, even minimal tissue disruption triggers inflammation and healing responses.
Targeted post-op care plans are designed to:
- Control inflammation early
- Protect healing tissues
- Reduce pain and swelling
- Prevent complications
- Promote faster functional recovery
When post-operative care is ignored or improperly followed, even a technically perfect procedure can result in delayed healing or unnecessary discomfort.
What Are Targeted Post-Op Care Plans?
Targeted post-vasectomy care plans are individualized recovery strategies based on patient risk factors, lifestyle, and procedural details. Instead of generic instructions, these plans consider:
- Activity level and occupation
- Pain sensitivity
- Prior scrotal or groin surgery
- Bleeding risk
- Anxiety level
- Medical history
By addressing these variables, targeted care plans optimize healing and improve patient satisfaction.
Immediate Post-Procedure Care (First 24 Hours)
The first 24 hours after no scalpel vasectomy are critical for preventing complications.
Scrotal Support and Positioning
Wearing snug, supportive underwear helps:
- Reduce tension on healing tissues
- Limit gravitational blood pooling
- Minimize swelling
Patients are often advised to rest with the scrotum elevated when lying down.
Cold Therapy Protocols
Targeted care plans specify:
- Ice application intervals (typically 15–20 minutes)
- Duration and frequency
- Protective layering to prevent skin injury
Cold therapy constricts blood vessels, reducing early bleeding and inflammation.
Activity Restriction
Rather than vague advice, targeted plans define:
- Maximum standing or walking time
- Avoidance of lifting thresholds
- Clear timelines for rest
This structured approach reduces the risk of hematoma formation.
Pain Management Tailored to the Patient
Pain levels after no scalpel vasectomy vary widely. Targeted post-op care plans use stepwise pain control rather than automatic medication use.
First-Line Pain Control
- Cold therapy
- Scrotal support
- Rest
These measures alone are sufficient for many patients.
Medication Strategies
When medication is needed, targeted plans may include:
- Short courses of NSAIDs
- Avoidance of aspirin during early recovery
- Clear dosing schedules
This minimizes side effects while maintaining comfort.
Swelling and Hematoma Prevention
Targeted care plans emphasize proactive management of swelling.
Compression-Based Strategies
- Continuous scrotal support during daytime
- Optional nighttime support for high-risk patients
Early Warning Education
Patients are taught to recognize:
- Rapid swelling
- Firm or tense scrotal areas
- Increasing pain despite rest
Early recognition allows timely intervention and prevents escalation.
Wound and Skin Care Without Incisions
Although no scalpel vasectomy does not involve incisions, skin care remains important.
Targeted plans include:
- Guidance on bathing timelines
- Keeping the puncture site clean and dry
- Avoidance of topical irritants
Because the puncture is small, most patients require minimal wound care, but instructions are still individualized.
Activity Progression and Lifestyle Integration
One of the most valuable aspects of targeted post-op care is structured activity progression.
Return to Daily Activities
Plans specify:
- When desk work is safe
- When walking distances can increase
- When driving can resume
Exercise and Physical Labor
Physically active patients receive clear timelines for:
- Light exercise
- Resistance training
- Sports participation
This prevents premature strain on healing tissues.
Sexual Activity and Fertility Safety
Targeted post-op care plans address sexual activity with clarity.
Timing Recommendations
Patients are advised on:
- When sexual activity can safely resume
- Expected sensations during early recovery
Semen Clearance Protocols
Targeted plans emphasize:
- Continued contraception use
- Follow-up semen analysis timelines
- Criteria for confirmed sterility
Clear guidance reduces anxiety and prevents unintended pregnancy.
Monitoring for Complications
A major advantage of targeted post-op care plans is structured monitoring.
Common Early Issues
Patients are educated about:
- Mild bruising
- Temporary soreness
- Minor swelling
When to Contact the Clinic
Clear thresholds are provided for:
- Increasing pain
- Fever or redness
- Rapid swelling
- Persistent discomfort
This proactive approach improves outcomes and reassurance.
Managing Anxiety and Expectations
Recovery is not only physical but psychological. Targeted care plans address patient concerns directly.
Strategies include:
- Clear explanation of normal healing sensations
- Written recovery timelines
- Access to follow-up support
Reducing uncertainty lowers stress and improves pain perception.
Special Populations and Customized Care
Certain patients benefit greatly from targeted post-op care.
Athletes and Physically Active Patients
Plans emphasize extended support use and delayed high-impact activity.
Patients With Prior Surgery
Care plans account for scar tissue and altered anatomy.
Patients With Bleeding Risks
More intensive monitoring and stricter activity limits may be used.
Role of Follow-Up Visits
Targeted post-op care plans integrate structured follow-up.
Follow-up allows clinicians to:
- Assess healing progress
- Address lingering discomfort
- Reinforce recovery guidance
- Adjust care plans if needed
This individualized oversight improves long-term satisfaction.
Long-Term Benefits of Targeted Post-Op Care
When post-operative care is personalized, patients experience:
- Faster recovery
- Lower complication rates
- Reduced chronic pain risk
- Higher confidence in the procedure
These benefits extend well beyond the immediate recovery period.
Future Trends in Post-Vasectomy Care
Innovation continues to enhance post-op management.
Emerging tools include:
- Telehealth-based recovery check-ins
- Wearable recovery trackers
- AI-driven risk stratification
- Digital care plan platforms
These advances will further refine targeted post-op care for no scalpel vasectomy patients.
Conclusion
No scalpel vasectomy and targeted post-op care plans together form a comprehensive approach to modern male sterilization. While the procedure itself minimizes tissue trauma, personalized post-operative care ensures optimal healing, comfort, and long-term outcomes.
By addressing individual risk factors, activity levels, and recovery needs, targeted care plans empower patients to heal confidently and avoid complications. As vasectomy care continues to evolve, personalized post-op strategies will remain a cornerstone of best-practice no scalpel vasectomy management.
FAQs
1. Why is targeted post-op care important after no scalpel vasectomy?
Targeted post-op care reduces complications, controls pain and swelling, and helps patients recover faster by tailoring guidance to individual needs.
2. How long should I strictly rest after no scalpel vasectomy?
Most patients benefit from 24–48 hours of focused rest, followed by gradual activity increase based on comfort and care plan guidance.
3. When should I contact my doctor during recovery?
Contact your doctor if you experience increasing pain, rapid swelling, fever, redness, or symptoms that worsen instead of improve.







Leave a Reply