Dendritic cell therapy represents a cutting-edge approach in immunotherapy, harnessing the body’s immune system to combat cancer and other diseases. This treatment involves extracting, modifying, and reintroducing specialized immune cells to enhance the body’s natural defenses against tumors. While success rates vary by cancer type and stage, clinical data shows promising outcomes, often ranging from 50-65% response rates in certain cancers like non-small cell lung cancer.
Cancer often evades traditional treatments like chemotherapy due to its ability to suppress immune responses. Dendritic cell therapy addresses this by training the immune system to recognize and attack tumor cells specifically, offering a targeted alternative or complement to conventional methods. Patients turn to it for its potential to extend survival and prevent recurrence, especially in advanced stages where standard therapies fall short.
This therapy gains traction because tumors create immunosuppressive environments, but activated dendritic cells can break through these barriers. For instance, in pancreatic cancer trials, it improved recurrence-free survival to 64% at two years. Its appeal lies in personalization, using a patient’s own cells to minimize rejection risks.
Several variations of dendritic cell therapy exist, tailored to specific needs. One common type uses monocyte-derived dendritic cells (MoDCs), cultured from blood with growth factors like GM-CSF and IL-4, then loaded with tumor antigens.
Another approach involves sipuleucel-T, an FDA-approved vaccine for prostate cancer, where dendritic cells are pulsed with prostatic acid phosphatase antigens. Emerging types include peptide-loaded or tumor lysate-pulsed dendritic cells, and next-generation versions combining them with checkpoint inhibitors for solid tumors. Clinics like those associated with longevity Frankfurt specialize in customized dendritic cell vaccines, often cryopreserved for repeated dosing.
Dendritic cell therapy stands out for its safety profile, with most side effects limited to mild fever, fatigue, or injection-site reactions. Unlike chemotherapy, it avoids drug resistance since it leverages the patient’s own cells, enabling sustained immune memory against cancer.
It excels at targeting metastases in hard-to-reach areas like lymph nodes or bones, where conventional drugs struggle. In multiple myeloma studies, it boosted four-year survival to 71% when combined with transplants. Additionally, its outpatient nature reduces hospital stays, making it feasible for ongoing care.
Patients experience prolonged survival, with trials showing 20% median overall survival increases across cancers. For non-small cell lung cancer stages III-IV, two-year survival reaches 60% versus 25-35% with standard care.
Dendritic cell therapy induces immune responses in 30-35% of cases, leading to tumor shrinkage or stabilization. It prevents recurrence by creating long-term T-cell memory, as seen in colon cancer where five-year disease-free survival hit 62.5%. Beyond oncology, longevity Frankfurt applications suggest anti-aging potential through immune rejuvenation.
Quality-of-life improvements include pain relief in 95% of advanced cervical cancer cases and better appetite or energy in 76-94% of treated patients.
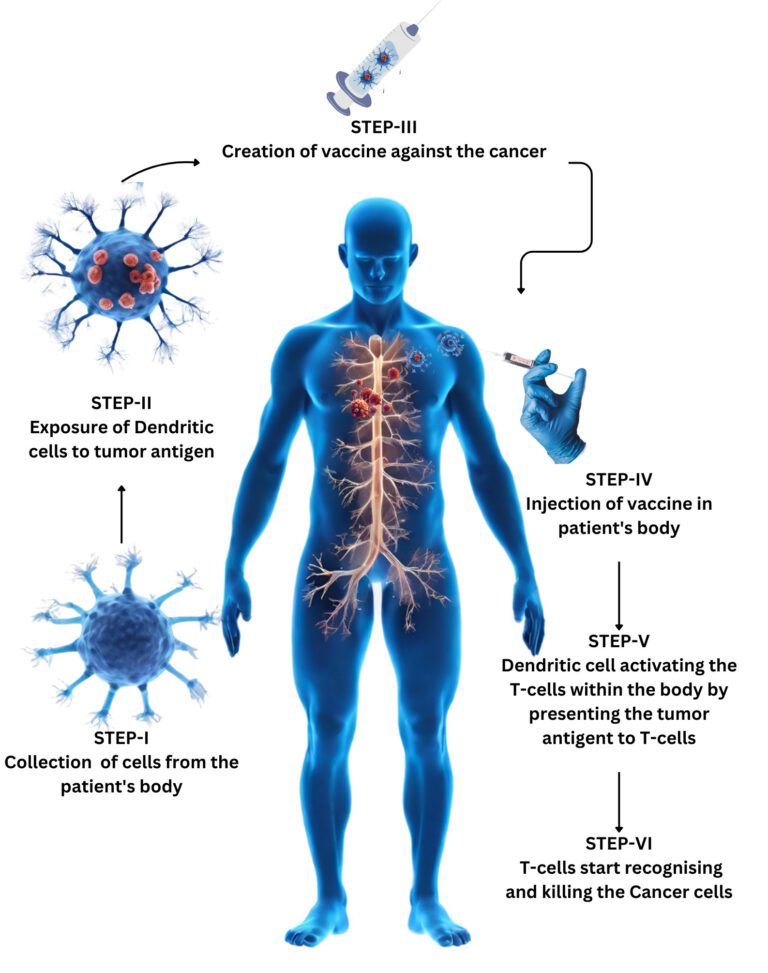
The process begins with leukapheresis, drawing blood to isolate monocytes, typically lasting 2-3 hours outpatient.
Next, lab cultivation differentiates monocytes into immature dendritic cells using cytokines, followed by maturation with tumor antigens like WT1 peptides or patient tumor lysates. This activation simulates infection, priming cells for immune attack over 5-7 days.
Quality checks ensure purity before reinfusion via subcutaneous injection near lymph nodes or tumors, often weekly for reinforcement. Monitoring follows, with possible cryopreservation for future doses; full cycles span 7-14 days.
Success varies: melanoma trials report 7-9% objective responses and 30% clinical benefit. Prostate cancer’s sipuleucel-T extended median survival by 3.9 months.
In NSCLC, 50-65% effectiveness includes tumor disappearance or stabilization. Pancreatic adjuvant therapy achieved 64% two-year recurrence-free survival. Longevity Frankfurt clinics report 50-65% efficacy, emphasizing survival over raw percentages. Overall, 60-85% immune activation correlates with better outcomes across studies.
Dendritic cell therapy offers hope for personalized cancer care, with evolving data supporting its role in improving survival and quality of life. Ongoing trials refine its application, particularly in combination regimens.
What cancers does dendritic cell therapy treat best?
Primarily prostate, melanoma, NSCLC, pancreatic, and glioblastoma, with best results in early or adjuvant settings.
How many sessions are needed?
Typically one comprehensive cycle with boosters; longevity Frankfurt protocols use single high-dose vaccinations cryopreserved for years.
Is it covered by insurance?
Often not, as it’s experimental in many regions, but available in specialized German clinics.[4]
What improves success rates?
Combination with surgery, chemo, or checkpoint inhibitors; patient health and antigen matching key factors. Any long-term side effects?
Rare; mostly mild and transient, with strong safety record over decades.
What cancers does dendritic cell therapy treat best?
Primarily prostate, melanoma, NSCLC, pancreatic, and glioblastoma, with best results in early or adjuvant settings.
How many sessions are needed?
Typically one comprehensive cycle with boosters; longevity Frankfurt protocols use single high-dose vaccinations cryopreserved for years.
Is it covered by insurance?
Often not, as it’s experimental in many regions, but available in specialized German clinics.[4]
What improves success rates?
Combination with surgery, chemo, or checkpoint inhibitors; patient health and antigen matching key factors.
Any long-term side effects?
Rare; mostly mild and transient, with strong safety record over decades.







Leave a Reply